P216: 39-year-old postpartum g3p2 heart transplant patient with rapid antibody response
(P216) 39-year-old postpartum g3p2 heart transplant patient with rapid antibody response
Location: Platinum Ballroom
Poster Presenter(s)
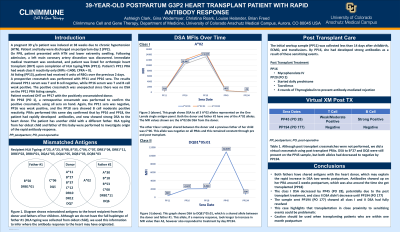
Body: A 39-year-old female (G3P2) was induced at 38 weeks due to chronic hypertension (HTN). She had an uneventful delivery, and patient and baby were discharged with no concerns on postpartum day 2 (PP2). On PP8, the patient presented with HTN and lower extremity swelling. Following admission for medical management, a left main coronary artery dissection was found. An emergent VAD was placed, followed by a 2 vessel CABG and ultimately ECMO placement on PP11 due to decompensation. The patient was listed for orthotopic heart transplant (OHT) and HLA typing/PRA was completed (PP11). At time of listing (PP13) the patient had received 4 units of RBCs over the previous 2 days. The patient’s initial PRA had weak class II reactivity only (MFIs <1400; cPRA = 0). The patient received an OHT on PP17. The prospective crossmatch (XM) was T cell and B cell weak positive using the sample from PP16, however the PP11 sample was T and B cell negative. A retrospective XM was performed the next day using pre-OHT and post-OHT serum samples to investigate the positive T cell prospective XM. Again, the sera from PP16 were T and B cell positive, whereas the serum from PP11 was T and B cell negative (Table 1). A PRA was performed on the PP16 and PP18 samples to compare with the initial sample drawn PP11. The CPRA increased from 0% to 87% from day PP11 to PP16, with DSA to A*02:06 (PP16, MFI = 10,447 and PP18, MFI = 13,169) and DQB1*05:01 (PP16, MFI = 2,027 and PP18, MFI= 2,066) (Table 1).
Conclusion: The initial workup sample was collected <14 days after childbirth, ECMO and transfusion. By PP17, she had developed strong antibodies as a result of these sensitizing events. Patient received mycophenolate IV starting day PP16, daily prednisone started PP20 (2 days post-OHT), and tacrolimus. Patient also received 4 rounds of Thymoglobulin (rabbit) to prevent rejection through 2 days post-OHT. Her husband is A*02:01P, which may explain the increase in antibodies two weeks postpartum, however we are unable to conclude what caused the class I DSA to decrease by day PP45. A post-transplant sample sent PP194 showed the DSA had fully resolved. This case highlights the issues surrounding transplant in close proximity to major sensitizing events. Caution should be used when transplanting patients who are within one month postpartum.
Conclusion: The initial workup sample was collected <14 days after childbirth, ECMO and transfusion. By PP17, she had developed strong antibodies as a result of these sensitizing events. Patient received mycophenolate IV starting day PP16, daily prednisone started PP20 (2 days post-OHT), and tacrolimus. Patient also received 4 rounds of Thymoglobulin (rabbit) to prevent rejection through 2 days post-OHT. Her husband is A*02:01P, which may explain the increase in antibodies two weeks postpartum, however we are unable to conclude what caused the class I DSA to decrease by day PP45. A post-transplant sample sent PP194 showed the DSA had fully resolved. This case highlights the issues surrounding transplant in close proximity to major sensitizing events. Caution should be used when transplanting patients who are within one month postpartum.

