(P207) Successful third transplant for recurrent leukemia after TLI-ATG conditioning and despite EBV-associated mixed donor chimerism.
Location: Platinum Ballroom
Poster Presenter(s)
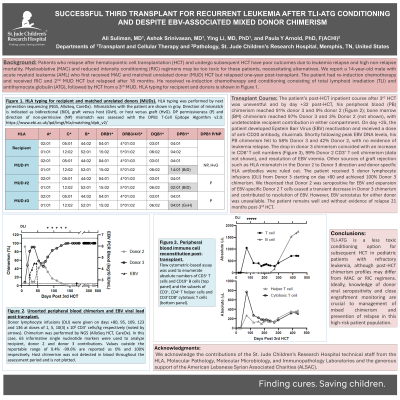
Body: Patients who relapse after hematopoietic cell transplantation (HCT) and undergo subsequent HCT have poor outcomes due to leukemia relapse and high non-relapse mortality. Myeloablative (MAC) and reduced intensity conditioning (RIC) regimens may be too toxic for these patients, necessitating alternatives. We report a 14-year-old male with acute myeloid leukemia (AML) who first received MAC and matched unrelated donor (MUD) HCT but relapsed one-year post-transplant. The patient had re-induction chemotherapy, and received RIC and 2nd MUD HCT but relapsed after 18 months. He received re-induction chemotherapy and conditioning consisting of total lymphoid irradiation (TLI) and antithymocyte globulin (ATG), followed by HCT from a 3rd MUD. The patient’s post-HCT inpatient course was uneventful and by day +32 post-HCT, his peripheral blood (PB) chimerism reached 91% donor 3 and 9% donor 2; bone marrow (BM) chimerism reached 97% Donor 3 and 3% Donor 2, with undetectable recipient contribution in either compartment. On day +25, the patient developed Epstein Barr Virus (EBV) reactivation, and received a dose of rituximab. Shortly following peak EBV DNA levels, his PB chimerism fell to 58% Donor 3 and 42% Donor 2, with no evidence of leukemia relapse. The drop in donor 3 chimerism coincided with an increase in CD8+ T cell numbers, 99% Donor 2 CD3+ T cell chimerism, and resolution of EBV viremia. Other sources of graft rejection such as HLA mismatch in the Donor 2 to Donor 3 direction and donor-specific HLA antibodies were ruled out. The patient received 5 donor lymphocyte infusions (DLI) from Donor 3 starting on day +80 and achieved 100% Donor 3 chimerism. We theorized that Donor 2 was seropositive for EBV and expansion of EBV-specific Donor 2 T cells caused a transient decrease in Donor 3 chimerism and contributed to resolution of EBV. However, EBV serostatus for either donor was unavailable. The patient remains well and without evidence of relapse 16 months post-3rd HCT.
Conclusion: TLI-ATG is a less toxic conditioning option for subsequent HCT in pediatric patients with refractory leukemia, although post-HCT chimerism profiles may differ from MAC or RIC regimens. Ideally, knowledge of donor viral seropositivity and close engraftment monitoring are crucial to management of mixed chimerism and prevention of relapse in this high-risk patient population.
Conclusion: TLI-ATG is a less toxic conditioning option for subsequent HCT in pediatric patients with refractory leukemia, although post-HCT chimerism profiles may differ from MAC or RIC regimens. Ideally, knowledge of donor viral seropositivity and close engraftment monitoring are crucial to management of mixed chimerism and prevention of relapse in this high-risk patient population.

