(P210) Donor specific antibodies to DQ antigens are rare in DR antigen matched kidney transplants
Location: Platinum Ballroom
Poster Presenter(s)
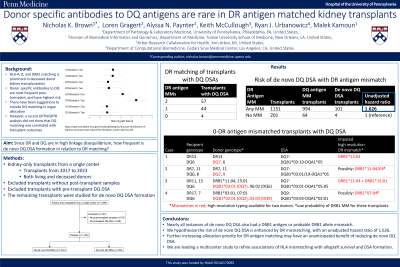
Aim: HLA-A, B and DR antigen matching is prioritized in the US deceased donor kidney allocation system, while HLA-DQ is the most frequent target of donor specific antibodies (DSAs) in kidney transplantation, and DQ DSAs are associated with poor outcomes. Therefore, recommendations have been made to include DQ matching in the allocation system. However, DR antigen matching was recently reported to be the only locus to be significantly associated with transplant outcomes in an OPTN analysis. Since DR and DQ loci are in high linkage disequilibrium, we sought to determine how frequent de novo DQ DSA is in relation to DR antigen matching.
Method: 1,499 kidney-only transplants between 2017 and 2023 from a single center were analyzed. Of these, 79 cases did not have any post-transplant antibody samples. 68 of the remaining transplants had pre-transplant DQ DSA and were removed from analysis; the remaining 1,352 transplants were analyzed for de novo DSA to either DQB1 or DQA1. Antigen-level mismatching was calculated for the DRB1 locus.
Results: 105 recipients developed de novo DQ DSA (7.8%). Of these cases, 57 had two DR antigen-level mismatches, 44 had one DR mismatch, and the remaining 4 transplants (3.8% of cases with DQ DSA) did not have a DR antigen mismatch (Fig. 1A). Three of the 4 cases of zero DR antigen mismatches developed DSA to DQ7, and one to DQ9 (Fig. 1B). The 4 cases of zero DR antigen mismatches were further analyzed with HLA imputation; two had at least one allele-level mismatch at DRB1, while imputation did not result in high confidence of a DRB1 mismatch for the other two. Any DR mismatch was found to have an unadjusted hazard ratio of 1.626 for risk of de novo DQ DSA development, compared to no DR antigen mismatch (Fig. 1C).
Conclusion: As nearly all instances of de novo DQ DSA also had a DRB1 antigen or probable DRB1 allele-level mismatch, we hypothesize that the risk of de novo DQ DSA is enhanced by DR mismatching. This is bolstered by the fact that a DR antigen mismatch was found to have an increased hazard ratio of de novo DQ DSA formation. Further increasing allocation priority for DR antigen matching may therefore have the unanticipated benefit of reducing de novo DQ DSA. A multicenter study is in progress that will help refine associations of HLA mismatching with allograft survival and DSA formation.
Method: 1,499 kidney-only transplants between 2017 and 2023 from a single center were analyzed. Of these, 79 cases did not have any post-transplant antibody samples. 68 of the remaining transplants had pre-transplant DQ DSA and were removed from analysis; the remaining 1,352 transplants were analyzed for de novo DSA to either DQB1 or DQA1. Antigen-level mismatching was calculated for the DRB1 locus.
Results: 105 recipients developed de novo DQ DSA (7.8%). Of these cases, 57 had two DR antigen-level mismatches, 44 had one DR mismatch, and the remaining 4 transplants (3.8% of cases with DQ DSA) did not have a DR antigen mismatch (Fig. 1A). Three of the 4 cases of zero DR antigen mismatches developed DSA to DQ7, and one to DQ9 (Fig. 1B). The 4 cases of zero DR antigen mismatches were further analyzed with HLA imputation; two had at least one allele-level mismatch at DRB1, while imputation did not result in high confidence of a DRB1 mismatch for the other two. Any DR mismatch was found to have an unadjusted hazard ratio of 1.626 for risk of de novo DQ DSA development, compared to no DR antigen mismatch (Fig. 1C).
Conclusion: As nearly all instances of de novo DQ DSA also had a DRB1 antigen or probable DRB1 allele-level mismatch, we hypothesize that the risk of de novo DQ DSA is enhanced by DR mismatching. This is bolstered by the fact that a DR antigen mismatch was found to have an increased hazard ratio of de novo DQ DSA formation. Further increasing allocation priority for DR antigen matching may therefore have the unanticipated benefit of reducing de novo DQ DSA. A multicenter study is in progress that will help refine associations of HLA mismatching with allograft survival and DSA formation.

