P211: Transplant outcomes in lung transplant candidates desensitized with a daratumumab based protocol
(P211) Transplant outcomes in lung transplant candidates desensitized with a daratumumab based protocol
Location: Platinum Ballroom
Poster Presenter(s)
Aim: Donor specific HLA antibodies (DSA) are associated with prolonged wait times and decreased allograft survival. Daratumumab is a CD38 monoclonal antibody used to deplete plasma cells. We aimed to evaluate the efficacy of a daratumumab based desensitization protocol could aid in getting highly sensitized critically ill lung transplant candidates transplanted and assess post-transplant outcomes.
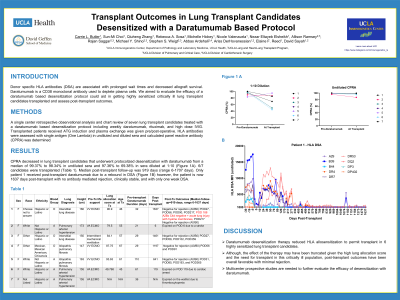
Method: A single center retrospective observational analysis and chart review of seven lung transplant candidates treated with a daratumumab based desensitization protocol including weekly daratumumab, rituximab, and high dose IVIG. Transplanted patients received ATG induction and plasma exchange was given pre/post-operative. HLA antibodies were assessed with single antigen (One Lambda) in undiluted and diluted sera and calculated panel reactive antibody (CPRA) was determined.
Results: CPRA decreased in lung transplant candidates that underwent protocolized desensitization with daratumumab from a median of 99.37% to 98.34% in undiluted sera and 97.36% to 69.38% in sera diluted at 1:10 (Figure 1A). 6/7 candidates were transplanted (Table 1). Median post-transplant follow-up was 919 days (range 6-1707 days). Only patient 1 received post-transplant daratumumab due to a rebound in DSA (Figure 1B) however, the patient is now 1637 days post-transplant with no antibody mediated rejection, clinically stable, and with only one weak DSA.
Conclusion: Daratumumab desensitization therapy reduced HLA allosensitization to permit transplant in 6 highly sensitized lung transplant candidates. Although, the effect of the therapy may have been truncated given the high lung allocation score and the need for transplant in this critically ill population, post-transplant outcomes have been overall favorable with minimal rejection. Multicenter prospective studies are needed to further evaluate the efficacy of desensitization with daratumumab.
Method: A single center retrospective observational analysis and chart review of seven lung transplant candidates treated with a daratumumab based desensitization protocol including weekly daratumumab, rituximab, and high dose IVIG. Transplanted patients received ATG induction and plasma exchange was given pre/post-operative. HLA antibodies were assessed with single antigen (One Lambda) in undiluted and diluted sera and calculated panel reactive antibody (CPRA) was determined.
Results: CPRA decreased in lung transplant candidates that underwent protocolized desensitization with daratumumab from a median of 99.37% to 98.34% in undiluted sera and 97.36% to 69.38% in sera diluted at 1:10 (Figure 1A). 6/7 candidates were transplanted (Table 1). Median post-transplant follow-up was 919 days (range 6-1707 days). Only patient 1 received post-transplant daratumumab due to a rebound in DSA (Figure 1B) however, the patient is now 1637 days post-transplant with no antibody mediated rejection, clinically stable, and with only one weak DSA.
Conclusion: Daratumumab desensitization therapy reduced HLA allosensitization to permit transplant in 6 highly sensitized lung transplant candidates. Although, the effect of the therapy may have been truncated given the high lung allocation score and the need for transplant in this critically ill population, post-transplant outcomes have been overall favorable with minimal rejection. Multicenter prospective studies are needed to further evaluate the efficacy of desensitization with daratumumab.

