(P213) Successful transplantation across high titer pre-existing donor-specific antibodies (DSA) in addition to cases involving de novo DSA with no antibody-mediated rejection
Location: Platinum Ballroom
Poster Presenter(s)
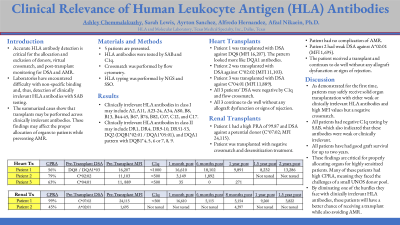
Body: Accurate Human Leukocyte Antigen (HLA) antibody interpretation is critical for allocation and exclusion of donors and post-transplant monitoring for donor-specific antibodies (DSA) and antibody-mediated rejection (AMR). The standard detection method is single antigen bead (SAB) analysis. However, clinical laboratories have encountered difficulties with non-specific binding and, thus, clinically irrelevant HLA antibodies. We investigated de novo DSA to HLA antigens in solid organ transplant recipients over the last decade, finding not all DSA to be clinically relevant or cause AMR. This helped us learn about clinically irrelevant antibodies and obtain good outcomes when transplanting the patients in our case study.
HLA typing was performed by Next Generation Sequencing (NGS) in all recipients and some donors. HLA antibody identification employed SAB testing, a semi-quantitative assay reporting antibody values as MFI. Complement component 1q (C1q) assay also evaluated antibody reactivity or strength. Monitoring renal and heart transplant outcomes in the last decade, we found that a good number of patients developed de novo DSA to HLA antigens with no indication of AMR. These are high-titer DSA with MFI = 10,0000 to >30,000. DSA have remained at persistent levels for years with negative biopsies and normal creatinine (renal). Most DSA were either against DR51- 53 or presumed to be DQA1. The nature of the reactivity is unclear. As previously suggested, they may be against denatured molecules, peptides associated with HLA antigens, or too weak for clinical significance.
This led us to transplant patients with pre-existing DSA to selective HLA antigens but negative C1q and crossmatch. Patients had smooth courses post-transplant with no increased DSA titer or AMR.
Conclusion: Our results show that not all SAB-detected DSA are clinically relevant or detrimental to allograft. Correlation of DSA to clinical outcome post-transplant may prevent unnecessary AMR treatment.
Furthermore, patients with pre-transplant existing DSA to selective antigens may be safely transplanted with thorough HLA investigation by C1q and crossmatch and close monitoring. These findings are critically significant for proper organ allocation to highly sensitized patients who have been on the transplant list for years or are severely ill.
HLA typing was performed by Next Generation Sequencing (NGS) in all recipients and some donors. HLA antibody identification employed SAB testing, a semi-quantitative assay reporting antibody values as MFI. Complement component 1q (C1q) assay also evaluated antibody reactivity or strength. Monitoring renal and heart transplant outcomes in the last decade, we found that a good number of patients developed de novo DSA to HLA antigens with no indication of AMR. These are high-titer DSA with MFI = 10,0000 to >30,000. DSA have remained at persistent levels for years with negative biopsies and normal creatinine (renal). Most DSA were either against DR51- 53 or presumed to be DQA1. The nature of the reactivity is unclear. As previously suggested, they may be against denatured molecules, peptides associated with HLA antigens, or too weak for clinical significance.
This led us to transplant patients with pre-existing DSA to selective HLA antigens but negative C1q and crossmatch. Patients had smooth courses post-transplant with no increased DSA titer or AMR.
Conclusion: Our results show that not all SAB-detected DSA are clinically relevant or detrimental to allograft. Correlation of DSA to clinical outcome post-transplant may prevent unnecessary AMR treatment.
Furthermore, patients with pre-transplant existing DSA to selective antigens may be safely transplanted with thorough HLA investigation by C1q and crossmatch and close monitoring. These findings are critically significant for proper organ allocation to highly sensitized patients who have been on the transplant list for years or are severely ill.

