Acute Heart Transplant Rejection in the Presence of Weak DSA with Negative Flow Cytometry Crossmatch
(P226) Acute heart transplant rejection in the presence of weak DSA with negative flow cytometry crossmatch
Location: Platinum Ballroom
Poster Presenter(s)
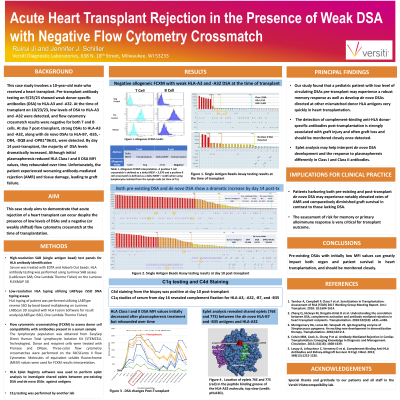
Body: This case study involves a 10-year-old male who received a heart transplant. Pre-transplant antibody testing on a 9/25/23 sample indicated only weak donor-specific antibodies (DSA) to HLA-A3 and -A32, and the clinical team chose to proceed with the organ offer. Single antigen bead testing at the time of transplant on 10/23/23 detected DSA to HLA-A3 (MFI=1,159) and -A32 (MFI=1,401) and Flow Cytometry Crossmatch (FCXM) results were both T cell and B cell negative. In contrast, FCXM with the historic sample were weakly T cell and B cell positive despite having similar DSA MFI values. Post-transplant the patient received blood products and underwent protocol immunosuppression. No Class I antibodies were detected and only a very low level of de novo HLA-DQ8 DSA was detected on day 4 post-transplant. However, by day 7 there were strong DSA to HLA-A3 and -A32 as well as de novo DSAs to HLA-B7, -B35, -DR4, and -DPB1*06:01. By day 10 there was a dramatic increase in DSA to HLA-A3 (MFI=25,303), -A32 (MFI=23,556), -B7 (MFI=21,503), and -B35 (MFI=26,162), along with a moderate increase in DSA to HLA-DR4 (MFI=11,564) and -DPB1*06:01 (MFI=18,824). C4d staining from the biopsy was positive at this time. On day 14 the clinical team initiated plasmapheresis. HLA Class I and II DSA MFI values initially decreased but rebounded over time (Fig. 1). C1q studies of serum from day 16 revealed complement fixation for HLA-A3, -A32, -B7, and -B35. The biopsy conducted on day 24 indicated a worsening in antibody-mediated rejection (AMR) accompanied by tissue damage. Eplet analysis revealed shared eplets (76ES and 77S) between the de novo HLA-B7 and -B35 antigens and HLA-A32, suggesting that de novo DSA development may contribute to stimulation of a memory response and may also help explain why the Class II DSA cleared faster during treatment.
Conclusion: This case highlights the importance of pre-existing DSAs with initially low MFI values, which can greatly impact both organ and patient survival. Individuals with circulating DSAs may experience a robust memory response as well as develop de novo DSAs directed at other mismatched donor HLA antigens very quickly. The detection of complement-binding anti-HLA donor-specific antibodies post-transplantation is strongly associated with graft injury and often graft loss, and should be monitored closely once detected.
Conclusion: This case highlights the importance of pre-existing DSAs with initially low MFI values, which can greatly impact both organ and patient survival. Individuals with circulating DSAs may experience a robust memory response as well as develop de novo DSAs directed at other mismatched donor HLA antigens very quickly. The detection of complement-binding anti-HLA donor-specific antibodies post-transplantation is strongly associated with graft injury and often graft loss, and should be monitored closely once detected.

