(P504) Haplo-Matched vs Haplo-Identical
Location: Platinum Ballroom
Poster Presenter(s)
Body: In Hematopoietic stem cell transplantation (HSCT), HLA identical siblings are preferred as donors because differences between polymorphic HLA antigens of donor-recipient pair stimulate alloimmune reactions causing graft-versus-host disease (GVHD) or graft rejection. HSCT from a haploidentical donor, however, is increasingly becoming a standard donor option for patients without a matched sibling or unrelated donor.
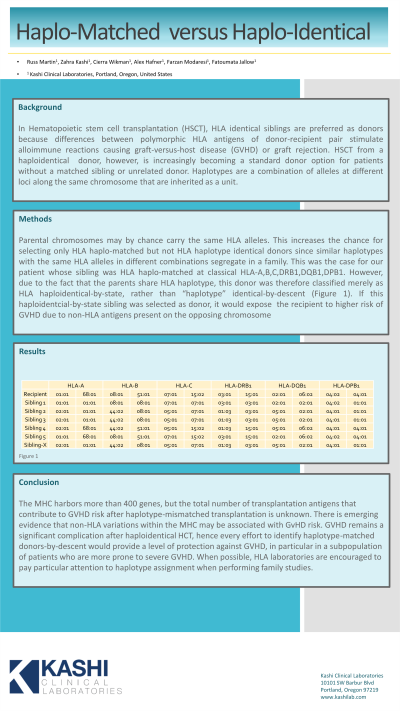
Haplotypes are a combination of alleles at different loci along the same chromosome that are inherited as a unit. Parental chromosomes may by chance carry the same HLA alleles. This increases the chance for selecting only HLA haplo-matched but not HLA haplotype identical donors since similar haplotypes with the same HLA alleles in different combinations segregate in a family. This was the case for our patient whose sibling was HLA haplo-matched at classical HLA-A,B,C, DRB1,DQB1,DPB1. However, due to the fact that the parents share HLA haplotype, this donor was therefore classified merely as HLA haploidentical-by-state, rather than “haplotype” identical-by-descent (Figure 1). If this haploidentcial-by-state sibling was selected as donor, it would expose the recipient to higher risk of GVHD due to non-HLA antigens present on the opposing chromosome.
Conclusion: The MHC harbors more than 400 genes, but the total number of transplantation antigens that contribute to GVHD risk after haplotype-mismatched transplantation is unknown. There is emerging evidence that non-HLA variations within the MHC may be associated with GvHD risk. GVHD remains a significant complication after haploidentical HCT, hence every effort to identify haplotype-matched donors-by-descent would provide a level of protection against GVHD, in particular in a subpopulation of patients who are more prone to severe GVHD. When possible, HLA laboratories are encouraged to pay particular attention to haplotype assignment when performing family studies.
Haplotypes are a combination of alleles at different loci along the same chromosome that are inherited as a unit. Parental chromosomes may by chance carry the same HLA alleles. This increases the chance for selecting only HLA haplo-matched but not HLA haplotype identical donors since similar haplotypes with the same HLA alleles in different combinations segregate in a family. This was the case for our patient whose sibling was HLA haplo-matched at classical HLA-A,B,C, DRB1,DQB1,DPB1. However, due to the fact that the parents share HLA haplotype, this donor was therefore classified merely as HLA haploidentical-by-state, rather than “haplotype” identical-by-descent (Figure 1). If this haploidentcial-by-state sibling was selected as donor, it would expose the recipient to higher risk of GVHD due to non-HLA antigens present on the opposing chromosome.
Conclusion: The MHC harbors more than 400 genes, but the total number of transplantation antigens that contribute to GVHD risk after haplotype-mismatched transplantation is unknown. There is emerging evidence that non-HLA variations within the MHC may be associated with GvHD risk. GVHD remains a significant complication after haploidentical HCT, hence every effort to identify haplotype-matched donors-by-descent would provide a level of protection against GVHD, in particular in a subpopulation of patients who are more prone to severe GVHD. When possible, HLA laboratories are encouraged to pay particular attention to haplotype assignment when performing family studies.