(P304) The reduction in immunosuppression laboratory dilemma
Location: Platinum Ballroom
Poster Presenter(s)
Body: Since the implementation of virtual crossmatch (vXM) February 2023 for all transplant wait list (TWL) recipients in Australia, new challenges have presented themselves to the tissue typing laboratories. While the issues are not new, the absence of a physical crossmatch at the time of deceased donor matching has put increased emphasis on the Luminex single antigen bead (SAB) assay results. Changes in immunosuppression treatment for retransplant renal recipients creates uncertainty in a vXM system.
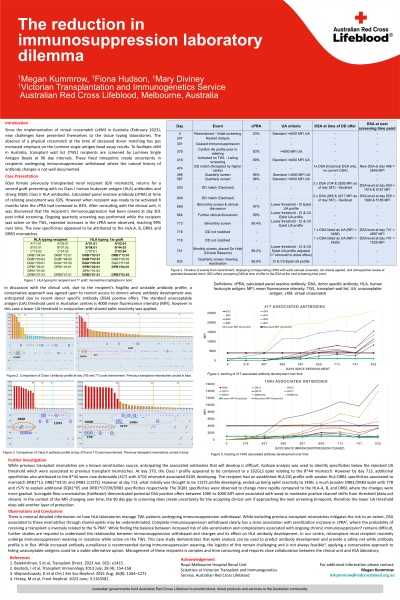
Previously transplanted renal recipient, returns for a second graft presenting with no Class I HLA antibodies and strong Class II HLA antibodies relating to the DQB1 previous transplant mismatch. Calculated PRA at time of relisting assessment was 63%. However when recipient was ready to be activated the cPRA had increased to 83%. The clinical unit was consulted to check potential sensitisation events, and it was discovered that the recipient’s immunosuppression had been ceased at day 308 post initial screening. Ongoing quarterly screening was performed while the recipient was active on the wait list, repeated increases were observed in the cPRA, antibody development attributed to the HLA-A, B, DRB1 and DRB3 mismatches.
Due to the developing antibodies and a quarterly screening schedule, the vXM at time of transplant offer may not reflect the recipient’s current antibody profile. In discussion with the treating unit, due to the recipient’s fragility and increasing antibody profile, a conservative approach was taken including increased frequency of screening and application lower threshold of donor specific antibody (DSA) acceptance. By using a lower threshold based on shared eplets, we were able to anticipate increases in MFI of alleles related to the transplant mismatches and this was confirmed by bi-monthly screening.
Conclusion: By using a more conservative approach by avoiding developing antibodies not yet at the routine unacceptable antigen level we were able to pre-emptively avoid high risk offers.
Previously transplanted renal recipient, returns for a second graft presenting with no Class I HLA antibodies and strong Class II HLA antibodies relating to the DQB1 previous transplant mismatch. Calculated PRA at time of relisting assessment was 63%. However when recipient was ready to be activated the cPRA had increased to 83%. The clinical unit was consulted to check potential sensitisation events, and it was discovered that the recipient’s immunosuppression had been ceased at day 308 post initial screening. Ongoing quarterly screening was performed while the recipient was active on the wait list, repeated increases were observed in the cPRA, antibody development attributed to the HLA-A, B, DRB1 and DRB3 mismatches.
Due to the developing antibodies and a quarterly screening schedule, the vXM at time of transplant offer may not reflect the recipient’s current antibody profile. In discussion with the treating unit, due to the recipient’s fragility and increasing antibody profile, a conservative approach was taken including increased frequency of screening and application lower threshold of donor specific antibody (DSA) acceptance. By using a lower threshold based on shared eplets, we were able to anticipate increases in MFI of alleles related to the transplant mismatches and this was confirmed by bi-monthly screening.
Conclusion: By using a more conservative approach by avoiding developing antibodies not yet at the routine unacceptable antigen level we were able to pre-emptively avoid high risk offers.

.jpeg)