Comparison of alloimmune risk stratification methods for kidney transplants: correlation with outcomes from a single center pediatric transplant program
(P310) Comparison of alloimmune risk stratification methods for kidney transplants
Location: Platinum Ballroom
Poster Presenter(s)
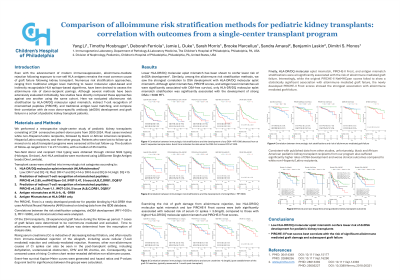
Aim: Even with the advancement of modern immunosuppression, exposure to non-self HLA antigens often results in the development of de novo donor-specific antibodies (dnDSAs), leading to chronic rejection and graft failure. Numerous risk stratification approaches, ranging from traditional antigen level matching to newer molecular eplet-based algorithms, have been devised to assess the alloimmune risk of donor-recipient pairings. Although several methods have been extensively evaluated individually, few studies have directly compared these approaches against one another using the same cohort. Here we compare the predictive power of several risk stratification method in a cohort of pediatric kidney transplant patients.
Method: We performed a retrospective single-center study of pediatric kidney transplants performed between 2008 and 2023. Two-field donor and recipient HLA typing was performed by NGS (Holotype, Omixon). Anti-HLA antibodies were monitored using LABScreen Single Antigen beads (One Lambda). Transplant cases were stratified into immunologic risk categories according to various parameters, including antigen-level mismatches at HLA-A/B/DR, molecular eplet mismatch (HLAMatchmaker), and indirect T-cell recognition of mismatched peptides (PIRCHE-II). Correlations between the risk stratification categories, dnDSA development, and clinical outcomes were evaluated.
Results: Among commonly utilized method, risk stratification based on HLA-DR/DQ single molecule eplet mismatch showed superior correlations with clinically significant dnDSA development and graft function compared to traditional risk stratification method based on antigen-level mismatches. Additionally, within this cohort, clinically significant dnDSAs were predominantly directed against HLA-DQ, and risk stratification based on HLA-DQ matching significantly correlated with dnDSA development and graft function.
Conclusion: Among commonly utilized immunologic risk assessment method. HLA-DR/DQ single molecule eplet mismatch risk stratification (openly available through NKR’s website) provides the best correlation with clinically significant dnDSA development and graft function based on our single-center pediatric kidney transplant cohort. Prioritizing matching at HLA-DR and -DQ over traditional matching at -A, -B, and -DR may improve transplant outcomes for pediatric patients.
Method: We performed a retrospective single-center study of pediatric kidney transplants performed between 2008 and 2023. Two-field donor and recipient HLA typing was performed by NGS (Holotype, Omixon). Anti-HLA antibodies were monitored using LABScreen Single Antigen beads (One Lambda). Transplant cases were stratified into immunologic risk categories according to various parameters, including antigen-level mismatches at HLA-A/B/DR, molecular eplet mismatch (HLAMatchmaker), and indirect T-cell recognition of mismatched peptides (PIRCHE-II). Correlations between the risk stratification categories, dnDSA development, and clinical outcomes were evaluated.
Results: Among commonly utilized method, risk stratification based on HLA-DR/DQ single molecule eplet mismatch showed superior correlations with clinically significant dnDSA development and graft function compared to traditional risk stratification method based on antigen-level mismatches. Additionally, within this cohort, clinically significant dnDSAs were predominantly directed against HLA-DQ, and risk stratification based on HLA-DQ matching significantly correlated with dnDSA development and graft function.
Conclusion: Among commonly utilized immunologic risk assessment method. HLA-DR/DQ single molecule eplet mismatch risk stratification (openly available through NKR’s website) provides the best correlation with clinically significant dnDSA development and graft function based on our single-center pediatric kidney transplant cohort. Prioritizing matching at HLA-DR and -DQ over traditional matching at -A, -B, and -DR may improve transplant outcomes for pediatric patients.