(P124) Novel null allele discovered by rapid next-gen sequencing
Location: Platinum Ballroom
Poster Presenter(s)
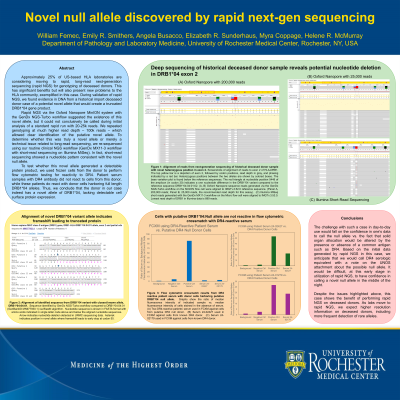
Body: Approximately 25% of US-based HLA laboratories are considering moving to rapid, long-read next-generation sequencing (rapid NGS) for genotyping of deceased donors. This has significant benefits but will also present new problems to the HLA community, exemplified in this case. During validation of rapid NGS, we found evidence in DNA from a historical import deceased donor case of a potential novel allele that would create a truncated DRB1*04 gene product.
Rapid NGS via the Oxford Nanopore MinION system with the GenDx NGS-Turbo workflow suggested the existence of this novel allele, but it could not conclusively be called during initial analysis of a standard rapid run with 20-25k reads. We repeated genotyping at much higher read depth – 100k reads – which allowed clear identification of the putative novel allele. To determine whether this was truly a novel allele or merely a technical issue related to long-read sequencing, we re-sequenced using our routine clinical NGS workflow (GenDx MX11-3 workflow with short-read sequencing on Illumina MiSeq). In fact, short-read sequencing showed a nucleotide pattern consistent with the novel null allele.
To test whether this novel allele generated a detectable protein product, we used frozen cells from the donor to perform flow cytometric testing for reactivity to DR4. Patient serum samples with DR4 antibody did not react to cells from this donor, while these patients do react with donor cells harboring full length DRB1*04 alleles. Thus, we conclude that the donor in our case indeed has a novel allele of DRB1*04, lacking detectable cell surface protein expression.
Conclusion: The challenge with such a case in day-to-day use would fall on the confidence in one’s data to call the null allele vs. the fact that solid organ allocation would be altered by the presence or absence of a common antigen such as DR4. Based on the initial data generated by rapid NGS in this case, we anticipate that we would call DR4 serologic equivalent with a note on the UNOS attachment about the possible null allele. It would be difficult, at this early stage in utilization of rapid NGS, to have confidence in calling a novel null allele in the middle of the night.
Despite the issues highlighted above, this case shows the benefit of performing rapid NGS on deceased donors. As labs move to rapid NGS, we expect higher resolution information on deceased donors, including more frequent detection of rare alleles.
Rapid NGS via the Oxford Nanopore MinION system with the GenDx NGS-Turbo workflow suggested the existence of this novel allele, but it could not conclusively be called during initial analysis of a standard rapid run with 20-25k reads. We repeated genotyping at much higher read depth – 100k reads – which allowed clear identification of the putative novel allele. To determine whether this was truly a novel allele or merely a technical issue related to long-read sequencing, we re-sequenced using our routine clinical NGS workflow (GenDx MX11-3 workflow with short-read sequencing on Illumina MiSeq). In fact, short-read sequencing showed a nucleotide pattern consistent with the novel null allele.
To test whether this novel allele generated a detectable protein product, we used frozen cells from the donor to perform flow cytometric testing for reactivity to DR4. Patient serum samples with DR4 antibody did not react to cells from this donor, while these patients do react with donor cells harboring full length DRB1*04 alleles. Thus, we conclude that the donor in our case indeed has a novel allele of DRB1*04, lacking detectable cell surface protein expression.
Conclusion: The challenge with such a case in day-to-day use would fall on the confidence in one’s data to call the null allele vs. the fact that solid organ allocation would be altered by the presence or absence of a common antigen such as DR4. Based on the initial data generated by rapid NGS in this case, we anticipate that we would call DR4 serologic equivalent with a note on the UNOS attachment about the possible null allele. It would be difficult, at this early stage in utilization of rapid NGS, to have confidence in calling a novel null allele in the middle of the night.
Despite the issues highlighted above, this case shows the benefit of performing rapid NGS on deceased donors. As labs move to rapid NGS, we expect higher resolution information on deceased donors, including more frequent detection of rare alleles.

