Exploring Bioinformatics Tools for Graft-Versus-Host Disease Risk Prediction in Hematopoietic Cell Transplantation: A Study Conducted at a Mexican Center
(P125) Exploring bioinformatics tools for graft-versus-host disease risk prediction in hematopoietic cell transplantation
Location: Platinum Ballroom
Poster Presenter(s)
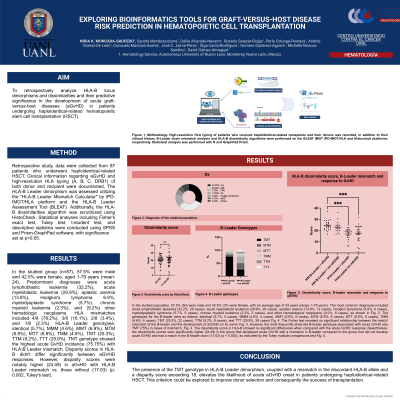
Aim: To retrospectively analyze HLA-B locus dimorphisms and dissimilarities and their predictive significance in the development of acute graft-versus-host diseases (GvHD) in patients undergoing haploidentical-related hematopoietic stem cell transplantation (HSCT).
Method: Retrospective study, data were collected from 87 patients who underwent haploidentical-related HSCT. Clinical information regarding GvHD and high-resolution HLA typing (A, B, C, DRB1) of both donor and recipient were documented. The HLA-B Leader dimorphism was assessed utilizing the "HLA-B Leader Mismatch Calculator" by IPD-IMGT/HLA platform and the HLA-B Leader Assessment Tool (BLEAT). Additionally, the HLA-B dissimilarities algorithm was scrutinized using HistoCheck. Statistical analyses including Fisher's exact test, Tukey test, t-student test, and descriptive statistics were conducted using SPSS and Prism-GraphPad software, with significance set at p<0.05.
Results: In the studied group (n=87), 57.5% were male and 42.5% were female, aged 1-79 years (mean: 24). Predominant diagnoses were acute lymphoblastic leukemia (32.2%), acute myeloblastic leukemia (29.9%), aplastic anemia (13.8%), Hodgkin's lymphoma 6.9%, myelodysplastic syndrome (5.7%), chronic myeloid leukemia (2.3%), and (9.2%) other hematologic neoplasms. HLA mismatches included 4/8 (78.2%), 3/8 (16.1%), 2/8 (3.4%), and 1/8 (2.3%). HLA-B Leader genotypes: identical (5.7%), MMM (4.6%), MMT (6.9%), MTM (6.9%), MTT (6.9%), TMM (4.6%), TMT (25.3%), TTM (9.2%), TTT (29.9%). TMT genotype showed the highest acute GvHD incidence (75.75%) with HLA-B Leader mismatch. Disparity scores in HLA-B didn't differ significantly between acute GVHD responses. However, disparity scores were notably higher (24.49) in acute GvHD with HLA-B Leader mismatch vs. those without (17.63) (p: 0.002, Tukey's test).
Conclusion: The presence of the TMT genotype in HLA-B Leader dimorphism, coupled with a mismatch in the discordant HLA-B allele and a disparity score exceeding 18, elevates the likelihood of acute GvHD onset in patients undergoing haploidentical-related HSCT. This criterion could be explored to improve donor selection and consequently the success of transplantation.
Method: Retrospective study, data were collected from 87 patients who underwent haploidentical-related HSCT. Clinical information regarding GvHD and high-resolution HLA typing (A, B, C, DRB1) of both donor and recipient were documented. The HLA-B Leader dimorphism was assessed utilizing the "HLA-B Leader Mismatch Calculator" by IPD-IMGT/HLA platform and the HLA-B Leader Assessment Tool (BLEAT). Additionally, the HLA-B dissimilarities algorithm was scrutinized using HistoCheck. Statistical analyses including Fisher's exact test, Tukey test, t-student test, and descriptive statistics were conducted using SPSS and Prism-GraphPad software, with significance set at p<0.05.
Results: In the studied group (n=87), 57.5% were male and 42.5% were female, aged 1-79 years (mean: 24). Predominant diagnoses were acute lymphoblastic leukemia (32.2%), acute myeloblastic leukemia (29.9%), aplastic anemia (13.8%), Hodgkin's lymphoma 6.9%, myelodysplastic syndrome (5.7%), chronic myeloid leukemia (2.3%), and (9.2%) other hematologic neoplasms. HLA mismatches included 4/8 (78.2%), 3/8 (16.1%), 2/8 (3.4%), and 1/8 (2.3%). HLA-B Leader genotypes: identical (5.7%), MMM (4.6%), MMT (6.9%), MTM (6.9%), MTT (6.9%), TMM (4.6%), TMT (25.3%), TTM (9.2%), TTT (29.9%). TMT genotype showed the highest acute GvHD incidence (75.75%) with HLA-B Leader mismatch. Disparity scores in HLA-B didn't differ significantly between acute GVHD responses. However, disparity scores were notably higher (24.49) in acute GvHD with HLA-B Leader mismatch vs. those without (17.63) (p: 0.002, Tukey's test).
Conclusion: The presence of the TMT genotype in HLA-B Leader dimorphism, coupled with a mismatch in the discordant HLA-B allele and a disparity score exceeding 18, elevates the likelihood of acute GvHD onset in patients undergoing haploidentical-related HSCT. This criterion could be explored to improve donor selection and consequently the success of transplantation.

