Precision in Post-Transplant Management: Revealing Epitope Mismatch Analysis for Enhanced Graft Survival Prediction
(P316) Precision in post-transplant management
Location: Platinum Ballroom
- EW
Poster Presenter(s)
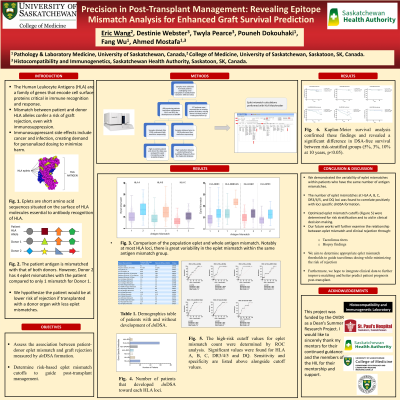
Aim: In the ever-changing landscape of transplantation and post-transplant management, there remains a demand for precise risk stratification and personalized treatment to minimize the side effects of immunosuppression. High-resolution HLA typing can be applied to analyze and evaluate patient and donor compatibility through epitope mismatch. Epitope mismatch is more descriptive than antigen mismatch and can potentially improve graft survival by improving matching and transplant management.
Method: To assess the relationship between epitope mismatch and graft survival, we used data collected from 626 patients monitored after renal transplantation in Saskatchewan. We examined the development of de novo DSA. Then, we used the Brazilian Eplet registry database to calculate eplet mismatches in HLA Matchmaker. High-resolution HLA data was obtained directly or predicted based on low-resolution typing through the HaploStats database.
Results: A wide range of eplet mismatch loads existed within the study population at each HLA locus (Figure 1). We found a significant correlation between eplet mismatch cut-offs and DSA formation and risk thresholds in HLA-A, B, C, and DQ (15, 11, 9, 9, p<0.05) (Figure 2). Subsequent Kaplan-Meier survival analysis confirmed these findings and revealed a significant difference in DSA-free survival between risk-stratified groups (5%, 3%, 10% at 10 years, p<0.05).
Conclusion: Epitope mismatch is a novel application of high-resolution sequencing with significant advantages over antigen mismatch. It can guide clinicians in determining risk and offer patients accurate prognoses. Integrating clinical data and further exploring the significance of specific epitopes can improve post-transplant management and patient care.
Method: To assess the relationship between epitope mismatch and graft survival, we used data collected from 626 patients monitored after renal transplantation in Saskatchewan. We examined the development of de novo DSA. Then, we used the Brazilian Eplet registry database to calculate eplet mismatches in HLA Matchmaker. High-resolution HLA data was obtained directly or predicted based on low-resolution typing through the HaploStats database.
Results: A wide range of eplet mismatch loads existed within the study population at each HLA locus (Figure 1). We found a significant correlation between eplet mismatch cut-offs and DSA formation and risk thresholds in HLA-A, B, C, and DQ (15, 11, 9, 9, p<0.05) (Figure 2). Subsequent Kaplan-Meier survival analysis confirmed these findings and revealed a significant difference in DSA-free survival between risk-stratified groups (5%, 3%, 10% at 10 years, p<0.05).
Conclusion: Epitope mismatch is a novel application of high-resolution sequencing with significant advantages over antigen mismatch. It can guide clinicians in determining risk and offer patients accurate prognoses. Integrating clinical data and further exploring the significance of specific epitopes can improve post-transplant management and patient care.
