The success of liver transplantation in patients with pre-transplant positive crossmatch depends on the liver’s ability to clear donor specific antibodies: A case study
(P323) The success of liver transplantation in patients with pre-transplant positive crossmatch depends on the liver’s ability to clear donor specific antibodies
Location: Platinum Ballroom
Poster Presenter(s)
Body: Liver transplantation is the definitive treatment for end-stage liver disease (ESLD). Positive pre-transplant crossmatch (XM) in the presence of donor-specific antibodies (DSAs) poses significant challenges to successful transplantation, especially if positive XM persists post-transplant.
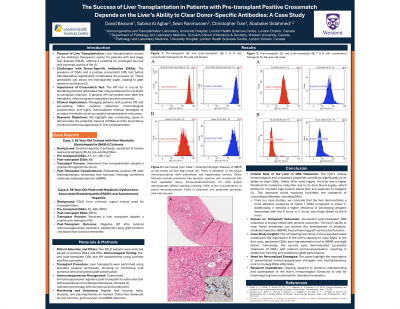
We report a case of a 55-year-old female with non-alcoholic steatohepatitis (NASH) cirrhosis and positive hepatitis C antibody. The patient was sensitized to human leukocyte antigens (HLA) and had detectable pre-existing DSAs. Despite a positive XM against the intended liver donor, the patient underwent transplantation. Post-transplant, the XM remained positive even after plasmapheresis, indicating unresolved DSAs (Fig-1). The patient’s liver function worsened, and histological examination revealed features consistent with antibody-mediated rejection (ABMR) Fig-3, underscoring the significance of a positive XM.
Conversely, a 58-year-old male with ESLD from cirrhosis due to metabolic associated steatohepatitis (MASH) and autoimmune hepatitis underwent liver transplantation due to urgent clinical needs despite a positive pre-transplant XM. Post-transplant, a tailored immunosuppressive regimen was initiated. Subsequent XM tests turned negative (Fig-2), suggesting resolved compatibility issues. The patient showed satisfactory early graft function and maintained stable liver function thereafter.
Conclusion: These cases underscore the liver’s critical role in clearing DSAs. Successful post-transplant DSA clearance is associated with positive outcomes, whereas failure to clear, indicated by persistently positive XM, typically results in poorer outcomes, as demonstrated in the first case. The cases also highlight the necessity for personalized immunosuppressive strategies and multidisciplinary collaboration, advanced immunological testing, and tailored immunosuppression regimens in managing patients with pre-existing DSAs and positive XMs. Continued research is essential to optimize desensitization protocols and enhance long-term graft outcomes for this high-risk population.
We report a case of a 55-year-old female with non-alcoholic steatohepatitis (NASH) cirrhosis and positive hepatitis C antibody. The patient was sensitized to human leukocyte antigens (HLA) and had detectable pre-existing DSAs. Despite a positive XM against the intended liver donor, the patient underwent transplantation. Post-transplant, the XM remained positive even after plasmapheresis, indicating unresolved DSAs (Fig-1). The patient’s liver function worsened, and histological examination revealed features consistent with antibody-mediated rejection (ABMR) Fig-3, underscoring the significance of a positive XM.
Conversely, a 58-year-old male with ESLD from cirrhosis due to metabolic associated steatohepatitis (MASH) and autoimmune hepatitis underwent liver transplantation due to urgent clinical needs despite a positive pre-transplant XM. Post-transplant, a tailored immunosuppressive regimen was initiated. Subsequent XM tests turned negative (Fig-2), suggesting resolved compatibility issues. The patient showed satisfactory early graft function and maintained stable liver function thereafter.
Conclusion: These cases underscore the liver’s critical role in clearing DSAs. Successful post-transplant DSA clearance is associated with positive outcomes, whereas failure to clear, indicated by persistently positive XM, typically results in poorer outcomes, as demonstrated in the first case. The cases also highlight the necessity for personalized immunosuppressive strategies and multidisciplinary collaboration, advanced immunological testing, and tailored immunosuppression regimens in managing patients with pre-existing DSAs and positive XMs. Continued research is essential to optimize desensitization protocols and enhance long-term graft outcomes for this high-risk population.

