(P407) HLA-DQ de novo donor-specific antibody development and its effect on renal allograft survival
Location: Platinum Ballroom
Poster Presenter(s)
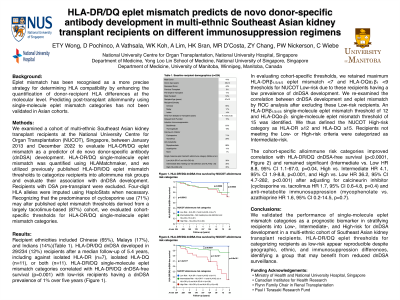
Aim: HLA-DQ are the most common de novo donor-specific antibodies (dnDSA) that develop post-transplantation and correlate with rejection and allograft loss. It is unknown whether the potential for HLA-DQ molecules to form cis- or trans-heterodimers affects the risk of dnDSA development or whether certain HLA-DQ allele mismatches are more immunogenic. We examined a large cohort of kidney transplant recipients to comprehensively evaluate the role of HLA-DQ trans-dimerization potential and specific HLA-DQ mismatches (in particular, DQα1*05 in combination with DQβ1*02:01/03:01 highlighted a previous report) on the risk of dnDSA development. We also examined the impact of HLA-DQ dnDSA on post-dnDSA allograft survival relative to dnDSA against other HLA loci.
Method: We analyzed 949 well-characterized renal transplant recipients for the relevance of cis/trans HLA-DQ molecules, specific HLA-DQ allele mismatches, eplet mismatch, and HLA-DQ dnDSA on allograft survival. Recipients were categorized into low, intermediate, and high-risk groups using previously published thresholds of HLA-DQ single molecule mismatch. Compatible HLA-DQ trans pairs were determined based on previously published research.
Results: Including potential cis/trans HLA-DQ mismatches did not improve HLA-DQ dnDSA prediction compared to cis HLA-DQ alone (AUC 0.76 vs. 0.77). However, maximum HLA-DQ eplet mismatch significantly correlated with dnDSA development (HR 1.11 per eplet mismatch, p<0.0001) independent of cis/trans HLA-DQ mismatch or specific HLA-DQ serologic groups. No specific HLA-DQ allele mismatches were statistically more likely to result in dnDSA development (Figure 1A), while alloimmune risk categories correlated with HLA-DQ dnDSA-free survival (p < 0.0001, Figure 1B). Recipients who developed HLA-DQ dnDSA had similar post-dnDSA death-censored allograft survival compared to recipients who developed Class I dnDSA (p=0.4, Figure 2A) and were less likely to progress to allograft loss compared to recipients who developed HLA-DR dnDSA (p=0.03) or HLA-DR and HLA-DQ dnDSA (p=0.02, Figure 2B).
Conclusion: HLA-DQ dnDSA development correlated best with eplet mismatch compared to specific HLA-DQ alleles. Although HLA-DQ dnDSA development was frequent, the more rapid progression to allograft loss associated with HLA-DR dnDSA highlights the need to consider both HLA-DR and HLA-DQ for alloimmune risk assessment strategies.
Method: We analyzed 949 well-characterized renal transplant recipients for the relevance of cis/trans HLA-DQ molecules, specific HLA-DQ allele mismatches, eplet mismatch, and HLA-DQ dnDSA on allograft survival. Recipients were categorized into low, intermediate, and high-risk groups using previously published thresholds of HLA-DQ single molecule mismatch. Compatible HLA-DQ trans pairs were determined based on previously published research.
Results: Including potential cis/trans HLA-DQ mismatches did not improve HLA-DQ dnDSA prediction compared to cis HLA-DQ alone (AUC 0.76 vs. 0.77). However, maximum HLA-DQ eplet mismatch significantly correlated with dnDSA development (HR 1.11 per eplet mismatch, p<0.0001) independent of cis/trans HLA-DQ mismatch or specific HLA-DQ serologic groups. No specific HLA-DQ allele mismatches were statistically more likely to result in dnDSA development (Figure 1A), while alloimmune risk categories correlated with HLA-DQ dnDSA-free survival (p < 0.0001, Figure 1B). Recipients who developed HLA-DQ dnDSA had similar post-dnDSA death-censored allograft survival compared to recipients who developed Class I dnDSA (p=0.4, Figure 2A) and were less likely to progress to allograft loss compared to recipients who developed HLA-DR dnDSA (p=0.03) or HLA-DR and HLA-DQ dnDSA (p=0.02, Figure 2B).
Conclusion: HLA-DQ dnDSA development correlated best with eplet mismatch compared to specific HLA-DQ alleles. Although HLA-DQ dnDSA development was frequent, the more rapid progression to allograft loss associated with HLA-DR dnDSA highlights the need to consider both HLA-DR and HLA-DQ for alloimmune risk assessment strategies.

