HLA-B*51:11N REVEALED BY NGS IN CONFIRMATORY DECEASED DONOR HLA TYPING
(P709) HLA-B*51
Location: Platinum Ballroom

Manli Shen, PhD
Jefferson Health
Poster Presenter(s)
Body: A deceased liver donor was re-typed by NGS at the Barnes-Jewish Hospital (BJH) HLA lab after the organ was transplanted, as the local standard of care to verify the deceased donor HLA typing and to facilitate donor-specific antibody (DSA) analysis at the allelic level. The donor was initially typed at a local OPO lab by real-time PCR using both LinkSeq and QTYPE assays. The HLA type reported at the time of organ allocation was A2, A3; B7 (Bw6), B51 (Bw4); Cw7, Cw7; DRB1*04:02, DRB1*11. The NGS typing at BJH was performed using the AllType 11-loci assay on the Ion Chef/Ion S5/TypeStream Visual platform, which showed a discrepant HLA-B genotype: B*07:02 (Bw6) and B*51:11N. All health metrics of the NGS typing were satisfactory.
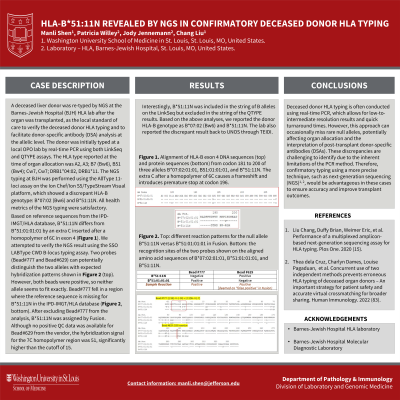
Based on reference sequences from the IPD-IMGT/HLA database, B*51:11N differs from B*51:01:01:01 by an extra C inserted after a homopolymer of 6C in exon 4 (Figure 1). We attempted to verify the NGS result using the SSO LABType CWD B-locus typing assay. Two probes (Bead#777 and Bead#629) can potentially distinguish the two alleles with expected hybridization patterns shown in Figure 2 (top). However, both beads were positive, so neither allele seems to fit exactly. Bead#777 fell in a region where the reference sequence is missing for the B*51:11N allele in the database (Figure 2, bottom). After excluding Bead#777 from the FUSION analysis, B*51:11N was assigned by the software. Although no positive QC data was available for Bead#629 from the vendor, the hybridization signal for the 7C homopolymer region was 51, significantly higher than the cutoff of 15. Interestingly, B*51:11N was included in the string of B alleles on the LinkSeq but excluded in the string of the QTYPE results. Based on the above analyses, we reported the donor HLA-B genotype as B*07:02 (Bw6) and B*51:11N. The lab also reported the B locus discrepancy to the UNET through TIEDI (Transplant Information Electronic Data Interchange).
Conclusion: Deceased donor HLA typing is frequently performed by real-time PCR and reported at low-to-intermediate resolution for a rapid turnaround time. Rare null alleles may be missed with these methods, which can impact the organ allocation and/or post-transplant DSA interpretation. Such errors are difficult to detect due to the method's limitations. Confirmatory typing using a more definitive method, such as NGS, would be beneficial in this setting.
Based on reference sequences from the IPD-IMGT/HLA database, B*51:11N differs from B*51:01:01:01 by an extra C inserted after a homopolymer of 6C in exon 4 (Figure 1). We attempted to verify the NGS result using the SSO LABType CWD B-locus typing assay. Two probes (Bead#777 and Bead#629) can potentially distinguish the two alleles with expected hybridization patterns shown in Figure 2 (top). However, both beads were positive, so neither allele seems to fit exactly. Bead#777 fell in a region where the reference sequence is missing for the B*51:11N allele in the database (Figure 2, bottom). After excluding Bead#777 from the FUSION analysis, B*51:11N was assigned by the software. Although no positive QC data was available for Bead#629 from the vendor, the hybridization signal for the 7C homopolymer region was 51, significantly higher than the cutoff of 15. Interestingly, B*51:11N was included in the string of B alleles on the LinkSeq but excluded in the string of the QTYPE results. Based on the above analyses, we reported the donor HLA-B genotype as B*07:02 (Bw6) and B*51:11N. The lab also reported the B locus discrepancy to the UNET through TIEDI (Transplant Information Electronic Data Interchange).
Conclusion: Deceased donor HLA typing is frequently performed by real-time PCR and reported at low-to-intermediate resolution for a rapid turnaround time. Rare null alleles may be missed with these methods, which can impact the organ allocation and/or post-transplant DSA interpretation. Such errors are difficult to detect due to the method's limitations. Confirmatory typing using a more definitive method, such as NGS, would be beneficial in this setting.
