Impact of the Virtual Crossmatch Assessment on Transplant Outcomes
(P206) Impact of the virtual crossmatch assessment on transplant outcomes
Location: Platinum Ballroom
Poster Presenter(s)
Aim: At our transplant center, the virtual crossmatch (VXM) assessment is used to proceed to kidney transplantation; therefore, its accuracy must be routinely confirmed. This study aims to compare the VXM assessment to results of physical flow cytometric crossmatch (FXM) and transplant outcomes.
Method: The VXM provides a risk assessment based on patient characteristics, HLA antibody relative strengths and shared epitopes, and a prediction of FXM. VXM is acceptable if the patient has a serum deemed current, absence of DSA or presence of low risk (1000-2000 MFI by Immucor single antigen) DSA, and no recent sensitization event. Acceptable VXMs are followed by a retrospective FXM (Halifaster protocol; cutoff ≥70MCS). VXMs are unacceptable and require a prospective FXM if the patient does not have a current specimen, has moderate risk (>2000 MFI) DSA present, had recent sensitizing events, or has a cPRA ≥ 80%.
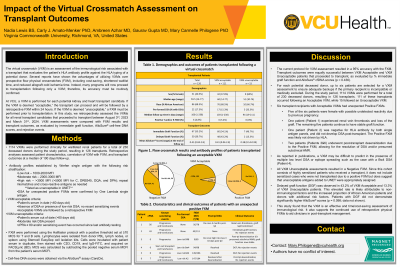
Results: Between August 3rd, 2023, and March 31st, 2024, 1114 VXMs were performed; 920 (82.6%) VXMs were deemed acceptable and 194 (17.4%) were deemed unacceptable. Of the acceptable VXMs, 111 (12.1%) proceeded to transplantation. Demographics and outcomes of those transplanted are listed in Table 1. Retrospective FXM were negative with T and B cells for 93.6% (103 of 110) of cases. Among the 7 unexpected positive flow crossmatches, 6 were sensitized against HLA antigens and 4 had pre-formed DSA <2000 MFI. Fifty four percent of the VXM acceptable cases had immediate graft function and 43.2% experienced delayed graft function (DGF). Within a median of 100 days post-transplant, donor-derived cell-free DNA, a presumed biomarker of rejection, showed a low-risk immunological complications (mean =0.41%) suggesting that the high rate of DGF was attributable to risk criteria rather than alloimmune rejection. No clinical indication biopsies were performed.
Of the 194 VXMs deemed unacceptable, 15 patients proceeded to transplant, 60% of which were female and 33.3% possessed pre-formed DSA shown insufficient to yield a positive FXM (0%). The 15 VXM unacceptable patients also showed minimal post-transplant dd-cfDNA scores (mean of 0.38).
Conclusion: Access to transplantation remains difficult for this complex patient population (68% AA, median age 59; significant rate of sensitization). Ongoing data analysis aims to identify predictive value of VXM for post-transplant DSA.
Method: The VXM provides a risk assessment based on patient characteristics, HLA antibody relative strengths and shared epitopes, and a prediction of FXM. VXM is acceptable if the patient has a serum deemed current, absence of DSA or presence of low risk (1000-2000 MFI by Immucor single antigen) DSA, and no recent sensitization event. Acceptable VXMs are followed by a retrospective FXM (Halifaster protocol; cutoff ≥70MCS). VXMs are unacceptable and require a prospective FXM if the patient does not have a current specimen, has moderate risk (>2000 MFI) DSA present, had recent sensitizing events, or has a cPRA ≥ 80%.
Results: Between August 3rd, 2023, and March 31st, 2024, 1114 VXMs were performed; 920 (82.6%) VXMs were deemed acceptable and 194 (17.4%) were deemed unacceptable. Of the acceptable VXMs, 111 (12.1%) proceeded to transplantation. Demographics and outcomes of those transplanted are listed in Table 1. Retrospective FXM were negative with T and B cells for 93.6% (103 of 110) of cases. Among the 7 unexpected positive flow crossmatches, 6 were sensitized against HLA antigens and 4 had pre-formed DSA <2000 MFI. Fifty four percent of the VXM acceptable cases had immediate graft function and 43.2% experienced delayed graft function (DGF). Within a median of 100 days post-transplant, donor-derived cell-free DNA, a presumed biomarker of rejection, showed a low-risk immunological complications (mean =0.41%) suggesting that the high rate of DGF was attributable to risk criteria rather than alloimmune rejection. No clinical indication biopsies were performed.
Of the 194 VXMs deemed unacceptable, 15 patients proceeded to transplant, 60% of which were female and 33.3% possessed pre-formed DSA shown insufficient to yield a positive FXM (0%). The 15 VXM unacceptable patients also showed minimal post-transplant dd-cfDNA scores (mean of 0.38).
Conclusion: Access to transplantation remains difficult for this complex patient population (68% AA, median age 59; significant rate of sensitization). Ongoing data analysis aims to identify predictive value of VXM for post-transplant DSA.

