(P224) Non-coding mismatches in HLA Class I genes in the presence of DPB1 mismatches predict worse outcomes in Hematopoietic Cell Transplantation
Location: Platinum Ballroom
Poster Presenter(s)
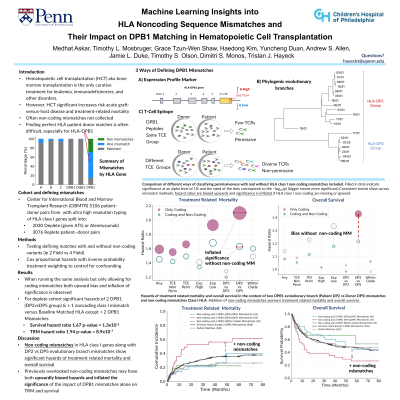
Aim: Hematopoietic cell transplantation (HCT) is vital for treating hematological malignancies. Recent studies recognize the potential impact of HLA-DPB1 mismatches on HCT outcomes, but a recombination hotspot makes matching HLA-DPB1 difficult. Therefore, current approaches attempt to find HLA-DPB1 mismatches that minimize risk. Furthermore, while matching on non-coding sequence has shown promise, the role of non-coding mismatches in the context of DP mismatches in HCT is unclear, necessitating further investigation. The first aim was to model different DPB1 mismatch scenarios and how they impact HCT outcomes, including: total DPB1 allele mismatches, T-cell epitope permissive versus non-permissive mismatches, high versus low expression, and mismatches across evolutionary clades. The second aim was to evaluate the impact of non-coding mismatches across class I HLA alleles on HCT outcomes in the context of these DPB1 mismatches.
Method: A retrospective study was performed with ultra-high resolution HLA typing in 5,109 HCT unrelated patient-donor pairs transplanted between 2008 and 2017 and reported to CIBMTR. The population included in vivo T-cell-depleted transplants (n = 2,030 patients received anti-thymocyte globulin or Alemtuzumab), and T-cell-replete transplants (n = 3,076), the two groups were analyzed separately. Weighted Cox proportional hazards models were employed to perform longitudinal analysis.
Results: Two HLA-DPB1 mismatches, using multiple criteria, lead to significant hazards of acute graft versus host disease grades 2 - 4, in the T cell replete group. In the T cell depleted group, increased hazards of both treatment related mortality (TRM) (HR=1.94, p-value=8.9x10-7) and overall survival (OS) (HR = 1.67, p-value = 1.3 x10-5) were observed when testing the additive effect of non-coding mismatches in the presence of two HLA-DPB1 mismatches, where the patient has a DP2 allele and the donor has a DP5 allele.
Conclusion: Elevated hazards of TRM and OS were associated with mismatches across evolutionary branches of HLA-DPB1 in conjunction with noncoding mismatches in class I HLA genes. In previous studies, unaccounted non-coding mismatches may have inflated the singular effect attributed to HLA-DPB1 mismatches. This emphasizes the need for comprehensive sequencing in HCT settings.
Method: A retrospective study was performed with ultra-high resolution HLA typing in 5,109 HCT unrelated patient-donor pairs transplanted between 2008 and 2017 and reported to CIBMTR. The population included in vivo T-cell-depleted transplants (n = 2,030 patients received anti-thymocyte globulin or Alemtuzumab), and T-cell-replete transplants (n = 3,076), the two groups were analyzed separately. Weighted Cox proportional hazards models were employed to perform longitudinal analysis.
Results: Two HLA-DPB1 mismatches, using multiple criteria, lead to significant hazards of acute graft versus host disease grades 2 - 4, in the T cell replete group. In the T cell depleted group, increased hazards of both treatment related mortality (TRM) (HR=1.94, p-value=8.9x10-7) and overall survival (OS) (HR = 1.67, p-value = 1.3 x10-5) were observed when testing the additive effect of non-coding mismatches in the presence of two HLA-DPB1 mismatches, where the patient has a DP2 allele and the donor has a DP5 allele.
Conclusion: Elevated hazards of TRM and OS were associated with mismatches across evolutionary branches of HLA-DPB1 in conjunction with noncoding mismatches in class I HLA genes. In previous studies, unaccounted non-coding mismatches may have inflated the singular effect attributed to HLA-DPB1 mismatches. This emphasizes the need for comprehensive sequencing in HCT settings.

