Triple Threat: Three Typing Assays Resulted Three Different HLA-DPB1 Typings
(P803) Triple threat
Location: Platinum Ballroom
- GC
Poster Presenter(s)
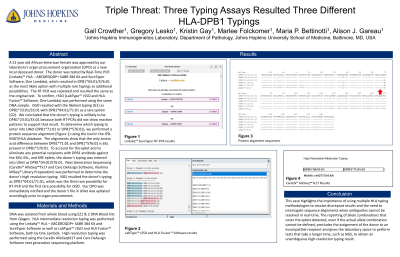
Body: A 52 year old African-American female was approved by our laboratory’s organ procurement organization (OPO) as a new local deceased donor. The donor was tested by Real-Time PCR (Linkseq™ HLA – ABCDRDQDP+ SABR 384 Kit and SureTyper Software, One Lambda), which resulted in DPB1*04:01/576:01 as the most likely option with multiple rare typings as additional possibilities. The RT-PCR was repeated and resulted the same as the original test. To confirm, rSSO (LabType™ rSSO and HLA Fusion™ Software, One Lambda) was performed using the same DNA sample. rSSO resulted with the likeliest typing (G1) as DPB1*23:01/33:01 with DPB1*04:01/71:01 as a rare option (G2). We concluded that the donor’s typing is unlikely to be DPB1*23:01/33:01 because both RT-PCRs did not show reaction patterns to support that result. To determine which typing to enter into UNet (DPB1*71:01 or DPB1*576:01), we performed a protein sequence alignment (Figure 1) using the tool in the IPD-IMGT/HLA database. The alignments show that the only amino acid difference between DPB1*71:01 and DPB1*576:01 is 65L present in DPB1*576:01. To account for this eplet and to eliminate any potential recipients with DPB1 antibody against the 36V, 65L, and 69E eplets, the donor’s typing was entered into UNet as DPB1*04:01/576:01. Next Generation Sequencing (CareDx® AlloSeq™Tx17 and Care DxAssign Software, Illumina MiSeq® Library Preparation) was performed to confirm the donor’s high resolution typing. NGS resulted the donor’s typing as DPB1*04:01/71:01, which was the third rare possibility for RT-PCR and the first rare possibility for rSSO. Our OPO was immediately notified and the donor’s file in UNet was updated accordingly prior to organ allocation.
Conclusion: This case highlights the importance of using multiple test methodologies to resolve discrepant results and the benefit of using sequence alignments to aid in the assignment of difficult typings.
Conclusion: This case highlights the importance of using multiple test methodologies to resolve discrepant results and the benefit of using sequence alignments to aid in the assignment of difficult typings.
