(P509) Refining HLA-associated type 1 diabetes risk assessment with data from six understudied countries
Location: Platinum Ballroom

Janelle Noble, PhD
UCSF
Poster Presenter(s)
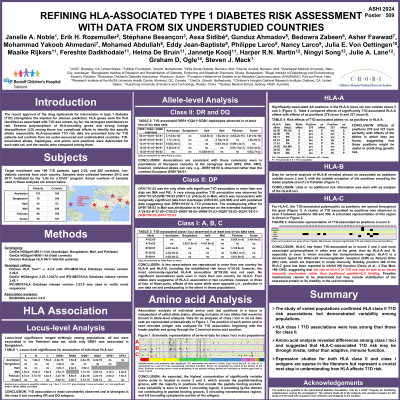
Aim: The HLA region is the primary contributor to type 1 diabetes (T1D) risk. This study was designed to assess HLA-associated T1D risk in T1D patients and controls from six under-resourced and understudied countries and to compare results in populations with different genetic backgrounds. Analyses of alleles, haplotypes, amino acid positions, and amino acid motifs were performed for each dataset and compared among them.
Method: One hundred T1D patients and 200 controls from six countries (Azerbaijan, Bangladesh, Haiti, Mali, Pakistan, and Sudan) were genotyped for classical HLA loci with GenDx NGSgo®-MX11-3. Haiti patients were genotyped with Omixon Holotype HLA assays. Statistical analyses were performed with BIGDAWG software.
Results: Both commonalities and variations were observed among the datasets. Overall locus-level T1D association varied from significance only at DR- and DQ-encoding loci (Haiti, Sudan) to significance at all loci (Mali, Pakistan). Magnitude also varied widely, e.g., DRB1 locus association was strong in Pakistan (p = 8.5 x 10-15) but weak in Bangladesh (p = 0.03); different alleles drove risk for each country (DRB1*03:01 in Pakistan; DRB1*04:01 in Bangladesh). DR- and DQ-encoding alleles showed the same direction of effect (predisposing vs. protective) among populations; however, class I and DP-encoding alleles often showed different effects depending on context, e.g., DPB1*04:02 appeared strongly susceptible in Mali (OR 12.53) but protective in Azerbaijan (OR 0.63). For HLA-C, five alleles appeard significantly associated in two different data sets; however, four showed different effects between populations. Examining individual amino acid residues and amino acid motifs allowed use of sparse data that would otherwise be binned. In Haitian data, a particular motif of eight amino acid residues, seen in 8 different DQB1 alleles, showed strong association with T1D (OR 2.46). Inclusion of DPB1*13:01 in haplotype with the motif greatly increased the risk magnitude (OR 7.35).
Conclusion: Recent FDA approval of a disease-modifying intervention underscores the need for optimized prediction and differential diagnosis of T1D. This in-depth study of six distinct populations addresses the complexity of pinpointing the actual (vs. apparent) risk factors for HLA-associated T1D risk in all individuals. Improved assessment is needed to optimize resource allocation and disease management.
Method: One hundred T1D patients and 200 controls from six countries (Azerbaijan, Bangladesh, Haiti, Mali, Pakistan, and Sudan) were genotyped for classical HLA loci with GenDx NGSgo®-MX11-3. Haiti patients were genotyped with Omixon Holotype HLA assays. Statistical analyses were performed with BIGDAWG software.
Results: Both commonalities and variations were observed among the datasets. Overall locus-level T1D association varied from significance only at DR- and DQ-encoding loci (Haiti, Sudan) to significance at all loci (Mali, Pakistan). Magnitude also varied widely, e.g., DRB1 locus association was strong in Pakistan (p = 8.5 x 10-15) but weak in Bangladesh (p = 0.03); different alleles drove risk for each country (DRB1*03:01 in Pakistan; DRB1*04:01 in Bangladesh). DR- and DQ-encoding alleles showed the same direction of effect (predisposing vs. protective) among populations; however, class I and DP-encoding alleles often showed different effects depending on context, e.g., DPB1*04:02 appeared strongly susceptible in Mali (OR 12.53) but protective in Azerbaijan (OR 0.63). For HLA-C, five alleles appeard significantly associated in two different data sets; however, four showed different effects between populations. Examining individual amino acid residues and amino acid motifs allowed use of sparse data that would otherwise be binned. In Haitian data, a particular motif of eight amino acid residues, seen in 8 different DQB1 alleles, showed strong association with T1D (OR 2.46). Inclusion of DPB1*13:01 in haplotype with the motif greatly increased the risk magnitude (OR 7.35).
Conclusion: Recent FDA approval of a disease-modifying intervention underscores the need for optimized prediction and differential diagnosis of T1D. This in-depth study of six distinct populations addresses the complexity of pinpointing the actual (vs. apparent) risk factors for HLA-associated T1D risk in all individuals. Improved assessment is needed to optimize resource allocation and disease management.
