P503: Identification of Non-HLA autoantibodies associated with biopsy-proven rejection in kidney transplantation
(P503) Identification of Non-HLA autoantibodies associated with biopsy-proven rejection in kidney transplantation
Poster Presenter(s)
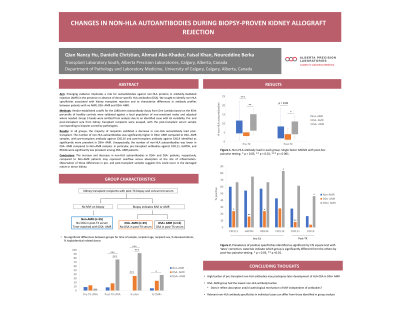
Aim: Emerging evidence implicates a role for autoantibodies against non-HLA proteins in antibody-mediated rejection (AMR) in the presence or absence of donor-specific HLA antibodies (HLA-DSA). We sought to identify non-HLA specificities associated with kidney transplant rejection and to characterize differences in antibody profiles between patients with no rejection (NR), HLA-DSA- AMR and HLA-DSA+ AMR.
Method: Vendor-established cutoffs based on the 85th percentile of healthy controls were validated against a local population of non-sensitized males and adjusted for certain beads as needed. Pre- and post-transplant sera from kidney transplant recipients were tested with the LABScreen Autoantibody Assay from One Lambda. Post-transplant sera correspond to biopsies indicating no rejection or suggestive of AMR as determined by pathologists.
Results: In the NR and HLA-DSA- AMR groups, the cumulative burden of non-HLA autoantibodies decreased post-transplant, whereas it was not significantly different to pre-transplant in the HLA-DSA+ AMR group. The number of non-HLA autoantibodies was significantly higher in HLA-DSA+ compared to HLA-DSA- samples both pre- and post-transplant. Unexpectedly, non-HLA autoantibodies were lower in HLA-DSA- AMR compared to NR samples, with pre-transplant PTPRN, AGRIN, and PRKCZ and post-transplant FLRT2 and IFNG being significantly less prevalent in the HLA-DSA- AMR group. Conversely, pre-transplant PRKCH and post-transplant CXCL9 were significantly enriched in HLA-DSA+ AMR compared to NR patients.
Conclusion: The increase and decrease in non-HLA autoantibodies in HLA-DSA+ and HLA-DSA- patients, respectively, compared to NR patients may represent overflow versus absorption at the site of inflammation. Observation of these differences in pre- and post-transplant samples suggests this could occur in the damaged native or donor kidney.
Method: Vendor-established cutoffs based on the 85th percentile of healthy controls were validated against a local population of non-sensitized males and adjusted for certain beads as needed. Pre- and post-transplant sera from kidney transplant recipients were tested with the LABScreen Autoantibody Assay from One Lambda. Post-transplant sera correspond to biopsies indicating no rejection or suggestive of AMR as determined by pathologists.
Results: In the NR and HLA-DSA- AMR groups, the cumulative burden of non-HLA autoantibodies decreased post-transplant, whereas it was not significantly different to pre-transplant in the HLA-DSA+ AMR group. The number of non-HLA autoantibodies was significantly higher in HLA-DSA+ compared to HLA-DSA- samples both pre- and post-transplant. Unexpectedly, non-HLA autoantibodies were lower in HLA-DSA- AMR compared to NR samples, with pre-transplant PTPRN, AGRIN, and PRKCZ and post-transplant FLRT2 and IFNG being significantly less prevalent in the HLA-DSA- AMR group. Conversely, pre-transplant PRKCH and post-transplant CXCL9 were significantly enriched in HLA-DSA+ AMR compared to NR patients.
Conclusion: The increase and decrease in non-HLA autoantibodies in HLA-DSA+ and HLA-DSA- patients, respectively, compared to NR patients may represent overflow versus absorption at the site of inflammation. Observation of these differences in pre- and post-transplant samples suggests this could occur in the damaged native or donor kidney.

